SCAD affects people from all walks of life in a variety of ways. The one thing we all have in common is that the experience of SCAD comes as a shock.
No-one expects to have a SCAD and, when it happens, it disrupts your plans: work, family, personal projects, and your sense of who you are and what is going on in your life. It would be very unusual if you didn’t also experience emotional upset, so you can expect that too.
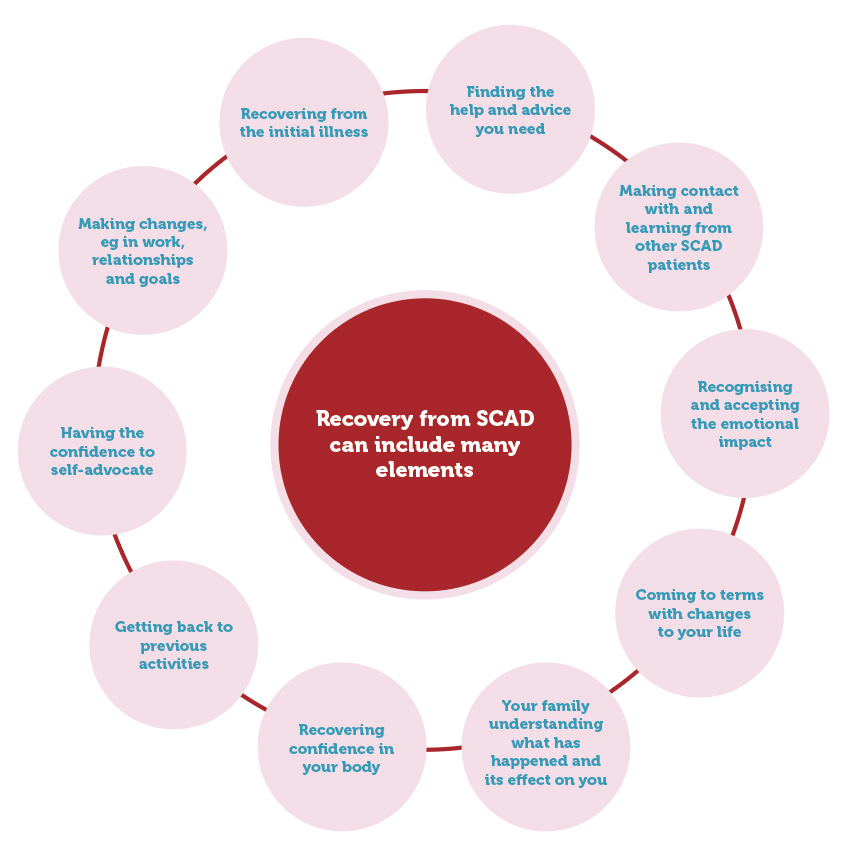
Everyone’s recovery is unique and is unlikely to be a linear process. It will involve some or all of the elements illustrated in this diagram.
Most people make a very good recovery from SCAD. However, it’s important to understand that recovery is both a physical and emotional journey and it’s going to take time. You cannot have your life turned on its head without going through a whole range of emotions.
At some point, you may experience many different emotions, including feeling lost, anxious, sad, angry or confused. You may doubt whether you can trust your own body and wonder about every little twinge of pain you get.
This is all part of understanding and adjusting to what has happened. Anyone who has a major health event is likely to go through these doubts and emotions and they are an important part of how you adapt and change to your circumstances.
Cardiac rehabilitation, good advice from your healthcare professionals, and support from the SCAD community will help you and your family on your journey to recovery.
There may be other sources of support that are also relevant to your needs or circumstances and the information on this website will help you to identify what those needs are.
Remember to be very kind to yourself and realise that recovery is a job that you need to learn how to do.
Browse the information in this section to discover what you can expect from Recovery, the Emotional Impact SCAD can have, Contraception and HRT, Pregnancy after SCAD, Finance and Travel.
We also offer some practical suggestions about what you can put into your SCAD Information Pack, what to consider when you want to Return to Work, and why it's important to Advocate for Yourself.
Emotional Impact
Many patients find the mental recovery can be harder than the physical one, so being aware of the Emotional impact of SCAD is important. And if you find your anxiety levels increasing, take a look at our suggestions and resources to help you Cope with Hypervigilance.
Families and friends can also be affected by SCAD and this page offers some advice.
Very sadly, some SCAD patients do not survive, so if you have lost a loved one, read our Bereavement page where there are resources that may help.
Recovery
In the Recovery section, there is information about
Living with SCAD...
Emotional Impact
Emotional and psychological recovery often takes longer than physical recovery, but there is help available
Emotional ImpactAdvocating for Yourself
Knowledge is power! SCAD is uncommon, so help your doctors to help you by becoming well informed
Advocating for YourselfSCAD Information Pack
Create a pack of information and documents to carry with you in case of emergency
SCAD Information PackReturning to Work
Hints and tips about what to consider when thinking about returning to work after a SCAD
Returning to WorkFor Patients...
What is SCAD?
Learn about Spontaneous Coronary Artery Dissection, who can be affected and how you can get support to help you on your post-SCAD journey
What is SCAD?Symptoms & Diagnosis
Understand the symptoms of SCAD, tests to diagnose it, genetic variants linked to SCAD and the chances of a recurrence
Symptoms & DiagnosisLiving with SCAD
This section discusses what your recovery might look like, the emotional impact of SCAD and practical things such as returning to work, travel and finances
Living with SCADSCAD Stories
Every SCAD patient’s experience is different, but you may find you relate to some of these stories
SCAD StoriesAssociated Conditions
Read about other diseases have been found to have an association with SCAD
Associated Conditions