SCAD causes heart attacks but looks different from atherosclerosis. It is important to consider a SCAD diagnosis where a patient looks very different from a ‘typical’ heart attack patient.
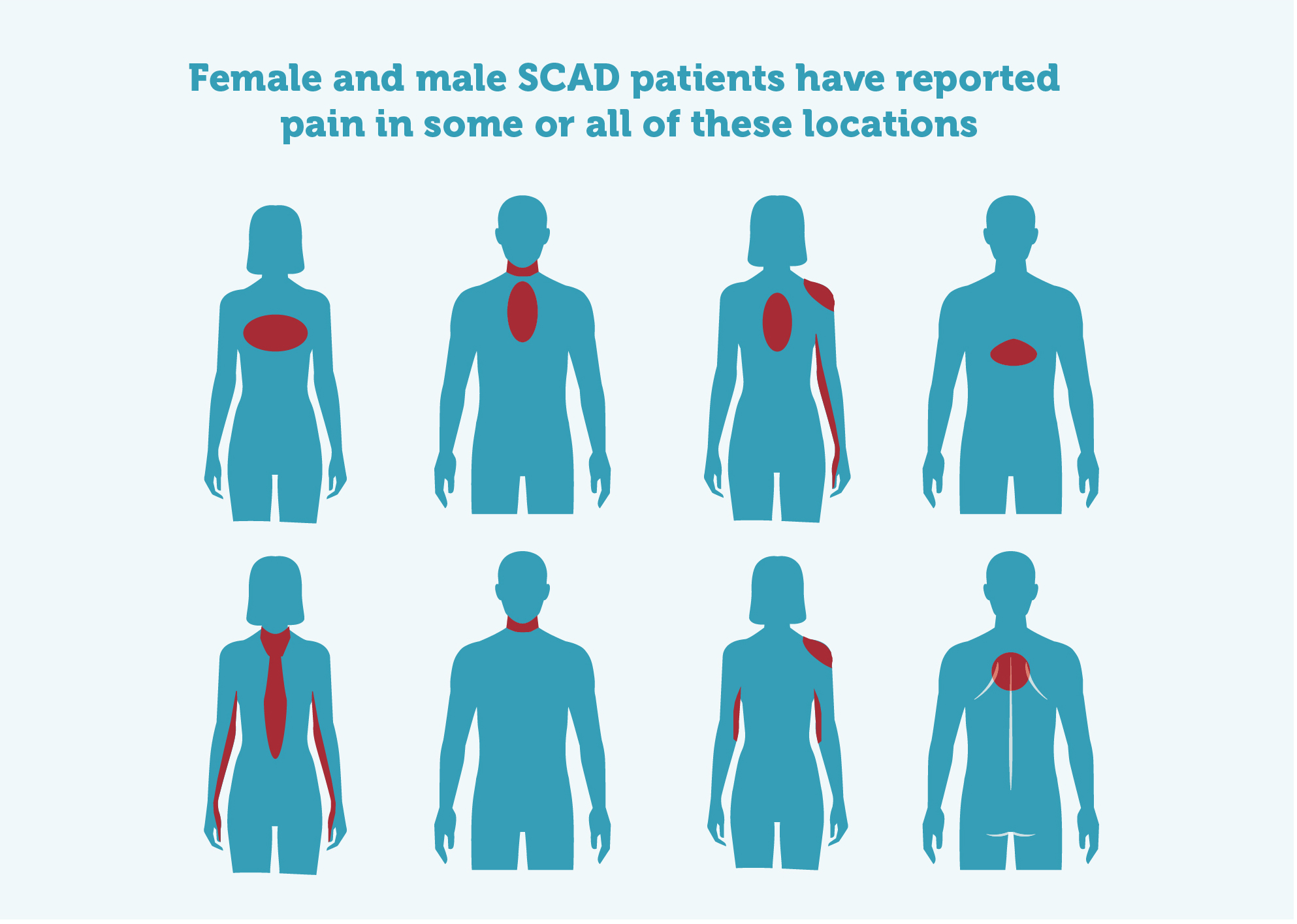
Typical symptoms*:
- Central chest pain
- Pain or numbness in one or both arms
- Jaw pain
- Back pain
- Shoulder pain
- Nausea
- Sweating/clamminess
- Difficulty breathing
- Some will have a sense of ‘impending doom’, others will try to convince themselves that their symptoms are anything but ACS
If your patient has possible cardiac symptoms, perform:
- ECG (may be normal)
- Troponin test (and repeat)
- Elevated Troponin: Consider angiography; be aware that SCAD does not always have the same appearance as iatrogenic coronary artery dissection.

Kate
Kate was working long hours and studying for a Masters when she had her SCAD, aged 52
Baseline measurement of Troponin levels, followed by serial measurements of Troponin a few hours later should be performed. Both the absolute value of the Troponin level as well as the degree of change in the Troponin level should be considered when diagnosing SCAD.
Women may experience a heart attack at a lower level of Troponin in the blood than men. A higher sensitivity Troponin blood test has been developed and is currently being tested.
٭ Remember, SCAD patients are often younger, more likely to be female and sometimes may have had a recent pregnancy. Atypical symptom presentations are more common in this patient population so consider a lower threshold for further investigations in hospital.
Some patients who had a SCAD during or after pregnancy offer their advice to healthcare professionals in this video.
Follow-up angiograms not recommended unless clinically needed
Follow-up invasive angiograms to check on healing are not recommended as there is a small risk of causing iatrogenic dissection with the catheters used during these procedures. However, recent studies show that virtually all SCADs heal by themselves between three and six months after the SCAD event.
Sometimes, if the SCAD is in the larger parts of the coronary arteries, a follow-up coronary CT scan can be done to confirm healing, but this is not a good option for SCADs that were in distal arteries as the spatial resolution of CT isn’t good enough to assess this with any accuracy. CT scans involve X-rays (with a small lifetime associated cancer risk) and in patients without symptoms, follow-up scans rarely highlight any important findings.
For patients with ongoing chest pain, a stress test (using imaging such as MRI or exercise) can be done to confirm there is no persisting issue with the blood supply to the heart.
For more see Risks and benefits of PCI intervention in SCAD
Post-SCAD Chest Pain Syndrome
60-90% of SCAD patients experience recurrent chest pain after SCAD (Post-SCAD Chest Pain Syndrome), according to studies referred to in the European Position Paper on SCAD.
Request Beat SCAD’s summary of the European Position Paper via the Downloads form.
Hospital readmission for chest pain after SCAD is also very common. Given the risk of recurrence (circa 10%), it is recommended that ECG and Troponin blood tests should always be done.
In some patients the pain is cyclical, usually pre-menstrual. Anecdotally, cyclical symptoms may respond to low-dose contraception (eg the progesterone hormonal Mirena Coil). For those who get non-cyclical spasm-like pain, vasodilator treatments may reduce vasospasms.
While the cause of post-SCAD chest pain is not fully understood, SCAD specialists recognise it and have observed that, over time, for most patients, it does get much better.
SCAD specialist Dr David Adlam said: “We don’t know why post-SCAD chest pain happens although there are some theories, such as a persistent tendency to have artery spasms or disruption of nerves in the heart that run along the side of vessels. Anything that damages nerves takes a long time to heal.”
Typically, for most patients, it will have faded into the background by 24 months (much sooner for many). However, a small number (much less than 10%) continue to experience chest pains longer than that.
Watch Dr Adlam discuss this video (starts at about 19 minutes).
Many patients also report experiencing strange sensations in their chests as they heal, which can be very concerning for them. These are often ectopic beats and palpitations. Dr Adlam talks about this from 41 minutes here.
Patients with prior pain syndromes or psychological or psychiatric disorders tend to be more at risk of Post-SCAD Chest Pain Syndrome and response to medication can be variable.
INOCA (Ischaemia with Non Obstructed Coronary Arteries) includes conditions such as Coronary Microvascular Dysfunction (Microvascular Angina), Coronary Artery Spasm and Takotsubo.
Like SCAD, INOCA conditions are often misunderstood and are also frequently under-recognised, under-diagnosed and under-treated.
For more information, see INOCA International.
Read more about current knowledge and emerging theories in the European Society of Cardiology SCAD Position Paper.
